| Home
About
|
Gout
Print-friendly version of this page
Posted by markferg@u.washington.edu, 7/12/04 at 11:25:23 AM.
Gout
What is it?
Gout is a form of peripheral arthritis resulting from the deposition of monosodium urate crystals secondary to hyperuricemia.
Prevalence in the United States: 1.6 to 13.6 per 1000
Typically occurs in middle aged or elderly males (90% of cases are in males).
It is particularly rare in premonpausal women.
Caucasians populations are more affected than those of African heritage.
Interestingly, gout is relatively frequent in young male Polynesians.
Hyperuricemia and gout are often associated with hypertension, obesity, hyperlipidemia, atherosclerosis, and ethanol abuse.
While
all gout patients have a high serum uric acid concentration at some
point in their disease progression, most hyperuricemic individuals
never show clinical signs of urate crystal deposition.
What causes it?
Uric acid under excretion (90% of cases)
Primary: Idiopathic reduced renal excretion
Secondary: Chronic renal failure
Thiazide use
Alcohol
Hyper or hypoparathyroidism
Uric acid overproduction (10% of cases)
Primary: Enzyme defect in purine synthesis
Secondary: Increased turnover of nucleic acids
Myeloproliferative and lymphoproliferative disorders
Hemolytic anemia
Chemotherapy
Alcohol
How does it present clinically?
The natural history of progressive urate crystal deposition manifests as three classic stages.
1. Acute gouty arthritis: 80% of attacks involve and single joint with severe pain,
redness, and swelling.
2.
Intercritical gout: These are asymptomatic intervals
between acute attacks most common early in
disease
progression. This pattern is quite uncommon in other arthritic
disorders
and alone is very suggestive of gout.
3. Chronic tophaceous gout: Collections of solid urate in connective tissues, which may be
calcified.
Attacks may occur for 4-6 years before radiographic evidence.
What are the radiographic features?
Location
Lower extremity > upper extremity
Small joints > large joints
Random distribution in hands (helpful diagnostic distinction)
First MTP most common (podagra)
Characteristics
Marginal, pararticular or intra-articular erosions which may
have overhanging edges
Well-defined erosions that may have a sclerotic border
Joint space preserved (unless very advanced)
Not usually associated with osteoporosis
Soft tissue and bursa deposition - tophi
MRI - Tophus has low intensity on T1 and variable low to high intensity on T2
depending on the
amount of amorphous calcification.
CT - Tophi have density similar to soft tissue.
Misc. Points
Erosions and tophi usually only with longstanding disease
40% of patients have concomitant CPPD
Can have many different appearances, but is quite common so always keep in mind.
Examples:

Shows classic location at first MTP and small erosion with
"overhanging" edge. Notice that the joint space and bone density are
preserved.

Another appearance showing multiple erosion locations including first
MTP, base of third and fourth metacarpals, and possibly the head of the
fifth metacarpal and second proximal phalanx.

Advanced gout resulting in joint destruction from large erosions in
first, fourth and fifth rays. Notice the large "overhanging" edges.

Example showing tophaceous gout of fifth MTP joint.

If you didn't appreciate the tophi on the last example, certainly you
will here. Notice calcification of the tophus on the ulnar side of
fifth MCP joint.

Patient with known gout. This example shows chondrocalcinosis of the
triangular fibrocartilage. 40% of gout patients have concomitant CPPD.
Also notice erosion of the head of the 5th proximal phalanx.
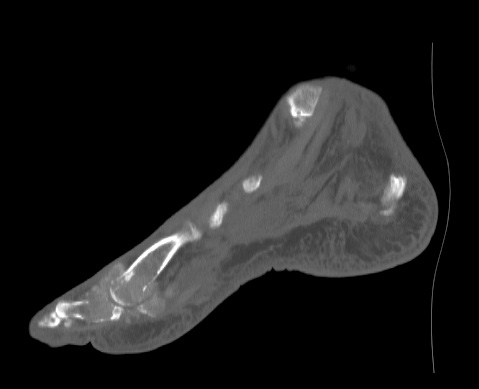 
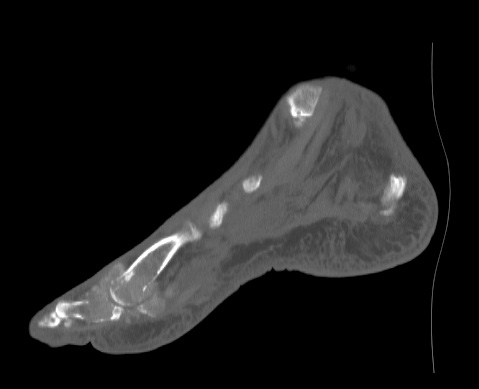
Tophaceous gout of the 1st MTP. Notice the tophi have a density similar
to soft tissue and are both inside and surrounding the bone. Also note
the cortical destruction of the proximal phalanx and the head of the
metacarpal.
Treatment
First line is to control associated disorders such as hypertension, obesity, hyperlipidemia, atherosclerosis, and ethanol abuse.
Acute attack - Goal is to quickly alleviate pain.
Anti-inflammatory therapy with NSAIDs, colchicine, or
Cox-2
inhibitors.
Should resolve symptoms in hours to days.
Prophylactic - Goal is to prevent acute attacks.
Indomethacin or colchicine.
In patients without evident
tophi,
prophylaxis can be safely discontinued 6 to 12 months after serum urate
levels
have
normalized.
Antihyperuricemic therapy - Goal is a serum urate concentration of 5 to 6 mg/dL which is
below that at
which monosodium urate is
saturating in extracellular fluids. Uricosuric
drugs and allopurinol can be used to lower the serum urate concentration.
Surgery
is typically only indicated to treat the complications of tophaceous
disease, which include infection, compression due to the mass effect of
a tophus, joint deformity, and intractable pain.
Tophaceous deposits may compress nerves or erode through the skin
resulting in chronic ulcers which often lead to infection.
1. Becker MA. Clinical manifestations and diagnosis of gout. UpToDate Version 12.2
2. Becker MA. Treatment of gout. UpToDate Version 12.2
3. Brant WE, Helms CA. Fundamentals of Diagnostic Radiology. 2nd ed. 1999 Lippincott Williams &
Wilkins Philadelphia.
4. Manaster BJ, Disler DG, May DA. Musculoskeletal imaging: the requisites. 2nd ed. 2002 Mosby,
Inc. St. Louis.
5. Ruddy et al. Kelley's Textbook of Rheumatology. 6th ed. 2001 W. B. Saunders Company
6. Weissleder R, Wittenberg J, Harisinghani MG. The Primer of Diagnostic Imaging. 3rd ed. 2003
Mosby, Inc. Philadelphia.
Discuss
|